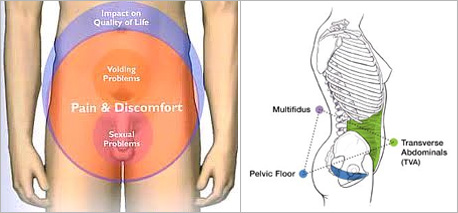
Pelvic Experts examine the trunk, abdomen, and pelvic anatomy. We assess functions of the male and female genitals, the surrounding pelvic tissues internally and externally. We also discuss all matters related to sexual health with each patient, to be sure your concerns are addressed. We identify if the whole body works in or out of balance. Body mechanics including how someone walks, sits, transitions, how someone works and play all make a difference in pain intensity and mobility. We analyze how the abdominal, spine, and pelvic floor work together and design and plan of treatment to help you improve.
- Abdominal pain
- Indigestion, gas, bloating
- Bowel and Bladder spasms
- Fecal and Urinary incontinence *** Read article: Uninary Incontinence in Women
- Fecal and Urinary retention
- Pelvic floor strengthening
- Pelvic pain/ Pelvic post surgeries
- Sacro-iliac dysfunction
- Sexual dysfunction
- Sexual pain
- Muscle spasms/ cramps
- Chronic Pelvic Pain
- Nerve compressions and many more…
Abdominal and Gastro-Intestinal Pain
The Digestive Tract is a long pipe made entirely of muscles and soft tissues. At each level there are different components of digestion taking place. The tract, made of smooth muscles, can contract/ relax to allow for normal motility and to facilitate the digestive process as food is moved down and converted to nutrition or to waste products. Any problems along the pipe is like "traffic jam", affecting normal flow and causing backed up, muscle spasms, reducing digestive function.
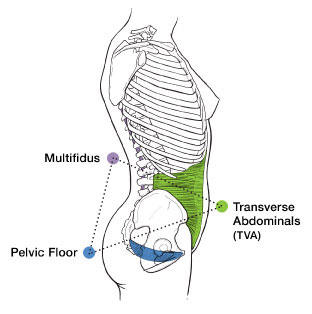
The Abdominal muscles are circumferentially wrapped around to protect the organs. They are voluntary muscles that contract/ relax along with the breathing diaphragm muscle on top, and pelvic floor muscles at the bottom. Often, we forget that we can use these muscles to compress and to expand for better flow of digestion and breathing. We can also use these muscles coordinating with pelvic floor contractions to improve control of our core and pelvic floor.
Gastro-Intestinal Problems, Indigestion, Bloating, frequent urination or bowel problems will place too much pressure onto the pelvic floor and genitals, which in turn can create pain and muscle spasm problems.
History of injury, trauma, dietary changes, life stresses, age, and health status, lack of exercise, and many more factors can create imbalance and weakness, inflammation, muscle atrophy, herniation, etc.
Pelvic Floor Rehabilitation (PFR) Table of Content:
- Summary of Action
- Anatomy
- Children's Pelvic Floor- Discussions of Problems in Children
- Women
- Men
- LGBT/ Transgender Issues
- Teens
- Prolapse
- Abdominal/Spine Considerations
- Pain
- Physical Disability
- Suggested Home Program
Summary of Action
Pelvic floor dysfunctions in children, men, and women are little discussed and or not well known. But there are solutions to help:- Don't feel isolated
- Don't accept your problem as permanent- there is always a solution when you look for it
- If you have pain or weakness in your low back, abdomen, and/or pelvic floor areas, they may be related to each other.
- If you or your child have a physical disability, consider problems with constipation, incontinence, back and pelvic pain and get treatment for them, they might not be able to tell you about these problems themselves.
- Refer yourself to practitioners who can help: get an appointment with a urologist, urogynecologist, gynecologist, or proctologist, and especially for physical therapists specializing in pelvic floor rehab, go online and do searches to find possible answers and referrals
- Always get second or third opinions if someone tells you nothing can be done
Anatomy
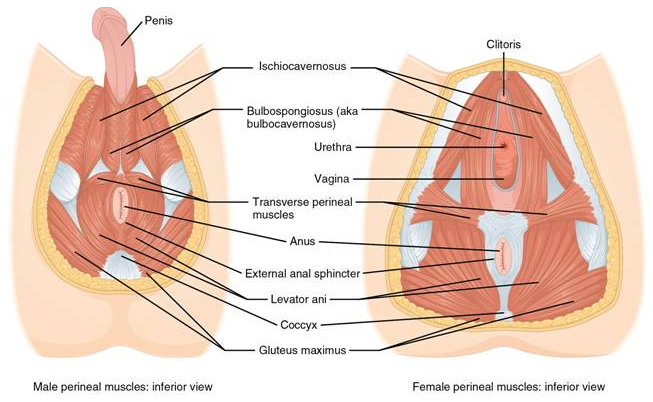
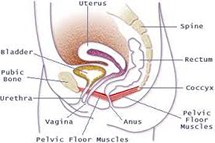
 The term Pelvic Floor refers to the entire area, including mostly muscles, and fascia, nerves, blood vessels surrounding the underside of the buttocks and pubic area. Front to back, it extends from the front where the pubic bones start, going around the 2 voiding areas, to the tip of the tail bone. Side to side it comes from attachments to the bones between the legs (Ischial tuberosities). The pelvic floor muscles are controlled voluntarily to lift up (contract) and relax. They look like a hammock with 2-3 openings for voiding. When a person wants to hold urine or feces, the "hammock" lifts up, and the muscles around the "pee" and "poo" contract. They relax down to allow voiding.
The term Pelvic Floor refers to the entire area, including mostly muscles, and fascia, nerves, blood vessels surrounding the underside of the buttocks and pubic area. Front to back, it extends from the front where the pubic bones start, going around the 2 voiding areas, to the tip of the tail bone. Side to side it comes from attachments to the bones between the legs (Ischial tuberosities). The pelvic floor muscles are controlled voluntarily to lift up (contract) and relax. They look like a hammock with 2-3 openings for voiding. When a person wants to hold urine or feces, the "hammock" lifts up, and the muscles around the "pee" and "poo" contract. They relax down to allow voiding.
In men, women, and children, control of the pelvic floor determines if they have normal voiding routine and hygiene or pain.
Children's Pelvic Floor Rehabilitation
In children, bladder or rectal training may have been delayed, or due to psychological, mental, social, or physical issues, bladder or rectal control is insufficient or missing.
 Children should not be scolded severely or physically punished when they are not able to control their voiding. Parents should consider all aspects of a child's physical function and behavior to determine how to train a child. Items to consider in cases of hard to train children are: health condition, including surgical history, height, weight, any other developmental delays (mental, cognitive, social, oral motor, fine and gross motor), social and family support, school system or daycare support. Besides behavioral and routine changes, a physical therapist should be consulted for voiding training. A urologist would check for any organ or physical dysfunction.
Children should not be scolded severely or physically punished when they are not able to control their voiding. Parents should consider all aspects of a child's physical function and behavior to determine how to train a child. Items to consider in cases of hard to train children are: health condition, including surgical history, height, weight, any other developmental delays (mental, cognitive, social, oral motor, fine and gross motor), social and family support, school system or daycare support. Besides behavioral and routine changes, a physical therapist should be consulted for voiding training. A urologist would check for any organ or physical dysfunction. Treatment is multi layered. Parents can keep a diary of voiding, intake, and behavior or atmosphere at the moment the child voids. Intake includes fluid (including any irritants), food, and medicine. A pattern might emerge to help the child. Manual feedback, stimulation, or massage will help relax areas of pain and tightness to allow the child to void properly. Exercises will help the child strengthen the pelvic floor (see appendix for exercises).
 Home programs may include use of devices such as biofeedback and electrical stimulation. Biofeedback first determines the weakness: if the child can hold a muscle contraction, how long is the hold (in seconds), how many reps can be repeated before fatigue, how quickly is the contraction. The child then can practice at home with the biofeedback unit. Electrical muscle stimulation devices can be used to help the muscles quickly contract and relax.
Home programs may include use of devices such as biofeedback and electrical stimulation. Biofeedback first determines the weakness: if the child can hold a muscle contraction, how long is the hold (in seconds), how many reps can be repeated before fatigue, how quickly is the contraction. The child then can practice at home with the biofeedback unit. Electrical muscle stimulation devices can be used to help the muscles quickly contract and relax. Note that problems are not always from weakness, but also from too much tightness. Example, a child who is so afraid of having accidents can also be holding too much, thus letting go when he or she is fatigued. So the pelvic floor training involves proper timing of contract/relax as appropriate.
Women's Pelvic Floor
In women and men, similar issues exist with leaking of urine and or feces or inability to hold flatulence. This is especially embarrassing in any society. PFR for incontinence in women involves discussions also of the menstrual cycle and how that might affect voiding and leakage. Any surgical procedures involving the female organ including removal of ovaries, uterus, insertion of slings, or birth of children (including episiotomy) might have stretched or torn the pelvic floor.
Home programs include pelvic floor exercises and or use of cones insertion to practice lifting or holding using the vaginal or rectal orifice.
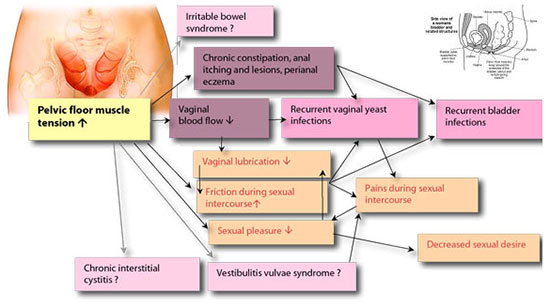
In women, pain from intercourse (dispareunia) can be treated as well. The vagina orifice might have muscle spasms and would not open sufficiently for intercourse, or the woman can feel severe pain just at the entrance of the vagina and cannot allow intercourse. This problem affects any sexual age and impedes normal sexual relationship, causing much anxiety and fear.
The pelvic floor and especially the vaginal orifice can be retrained to desensitize and allow opening at the right time. Training involves very calming, slow, self controlled stretching. The person can touch and self stretches with slow, calming breathing and using digital expansion. Overtime, even in a short period of time of a few weeks, this problem can be resolved. In women with compounded history of abuse or anxiety, it will take much more time, but it is possible to resolve these issues. Ask a physical therapist specializing in this treatment.Using cones or stretching rods with incremental sizes, biofeedback, muscle electrical stimulation may work.
Men
 In men, many problems can be addressed with exercises and self help. Surgeries and voiding patterns, prostate health or any other surgical procedures might affect the male organs and pelvic floor.
In men, many problems can be addressed with exercises and self help. Surgeries and voiding patterns, prostate health or any other surgical procedures might affect the male organs and pelvic floor.
Treatment for men would involve approaches to the area between the penis and the rectum, or inside the rectum. Problems of erectile dysfunction, especially after surgical procedures, can improve with electrical muscle stimulation and biofeedback.
LGBT/ Transgender Issues
We are aware of LGBT issues and related social, physical and emotional ramifications. We keep an open communication to be sure that all worries and concerns, questions are addressed.Transgenders have a special set of worries, including changes in anatomy, functional adaptation, and other physical and mental health stresses. We work with you to figure out causes of problems, help treat for pain, improve function, and nourish mental and physical health, reducing anxiety associated with acute and long term/ chronic problems.
Teens
Teens have a unique problem of being in the middle of childhood and adulthood. A lot of issues teens are shy to discuss their problem. They might not even realize that they have pelvic health problems. They might not want to talk about problems of incontinence, pain, sexual health, etc. Furthermore, they night be shy to have someone examine them. We gently work with each person to help improve trust, clarify situations, explaining the need to have issues addressed now to prevent future or compounded problems.Prolapse
In both women and men, there are also issues of organ prolapse- the rectum can protrude outside of the anal cavity especially during pushing with voiding. In women, because of the vaginal space, the bladder or rectum can sink into the vaginal walls. In these cases, a pessary or sling, or surgery may be needed to contain the problem.Abdominal and Spine Considerations
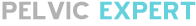
Many times, there might be pain in the pelvic floor without problems relating to continence. A person can have pain with the muscles and soft tissue inside or outside the pelvic floor. There are many causes of pelvic pain in women and men, including bladder infections, irritable bowels, pelvic inflammatory diseases, uterine fibroids, scar tissue adhesions, urinary tract infections, vulvodynia (pain with intercourse). Many problems will develop trigger pain, referring pain out to the pelvic floor, low back, and abdomen.
Pain
Pain in the low back and abdomen also refer to the pelvic floor. Any problems in the legs and feet may cause muscle guarding, pain reactions, holding patterns, postures that will affect pelvic floor functions. Any poor postures from the head, shoulders, spine, can result in abnormal holding of the pelvic and spine area. Therefore, when someone has problems, all aspects of a person must be considered. Pain treatment is determined by the source of the problem as well as treating local symptoms.Physical Disability
Do not forget patients with an existing physical disability. Many are born with muscle tone spasticity or flaccidity. Some patients become disable later in life such as spinal cord or head injury, or stroke, etc. They have special continence, pain, voiding issues that might need more intervention and medications to help.Summary of home programs:
- Start a log of voiding pattern, pain, what you are doing during this time
- Start a general exercise routine including movements of arms, legs, trunk, pelvis
- Focus more on pelvic floor exercises – ask a physical therapist pelvic floor specialist for correct techniques
- Massage belly and back, pelvic floor
- Use heating pads to help
- Find time during the day for quiet and relaxation (calming of tension) at least 5-10 minutes
- Work on deep diaphragmatic breathing with exhalation and relaxation
- Check your posture for good alignment
- Look into biofeedback or electrical stimulation if exercises do not help sufficiently
- Ask your doctors, including a good urologist, urogynecologist, gynecologist, and physical therapist who specialize in pelvic floor rehab and pain treatment.